
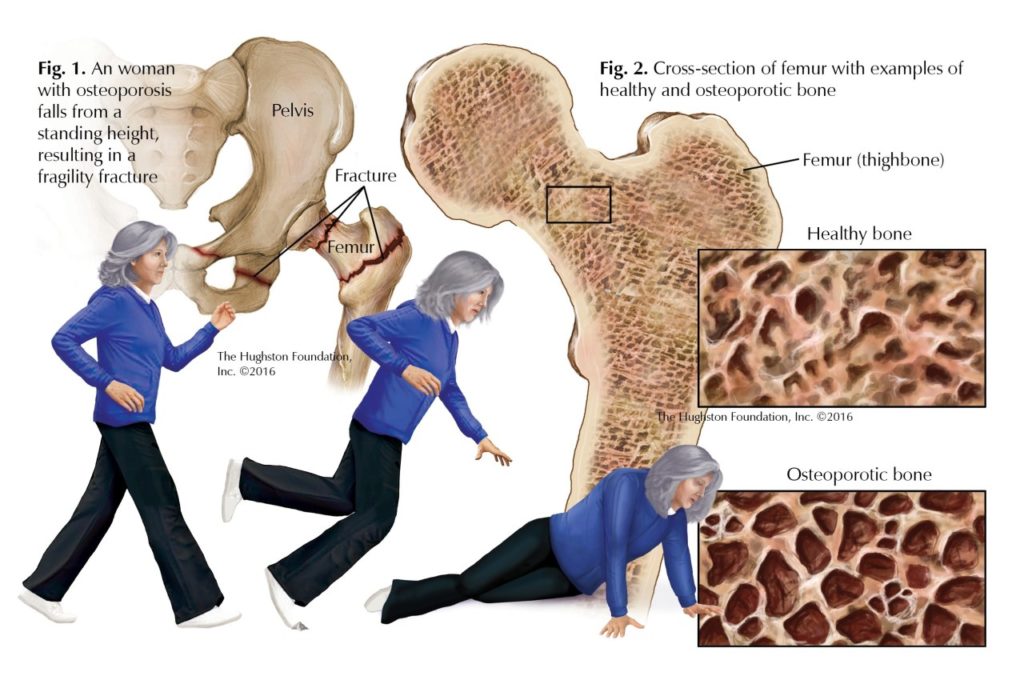
If you are over the age of 50, especially if you are also female, you may be at risk for a fragility fracture. The American Academy of Orthopaedic Surgeons defines fragility fractures as fractures that result from a fall from a standing height or that occur in the absence of obvious trauma (Fig. 1). These types of fractures affect up to 50% of all women and 25 to 33% of all men over 50 and are often due to low bone-mineral density. The hip, spine, and wrist are the most common sites where you could sustain a fragility fracture.
What causes fragility fractures?
Low-energy fragility fractures usually occur as a result of not just general low bone density, but the presence of osteoporosis. Osteoporosis is a bone disease characterized by the structural deterioration of both the inner and outer bone tissue, resulting in porous bones (Fig. 2). These changes lead to overall low bone mass, compromised bone strength, and an increased risk for fractures. If you do have osteoporosis, you are not alone: the National Osteoporosis Foundation estimates that 10 million people in the United States suffer from osteoporosis while another 34 million are at an increased risk of bone fracture due to osteopenia or low bone mass. One of the most serious injuries you can suffer as a result of osteoporosis is a hip fracture; 50% of those who suffer a hip fracture will lose the ability to live independently.
Additional risk factors
Once you have suffered a fragility fracture, you have a greater risk of sustaining another. Apart from age, gender, and a previous fracture, risk factors include a family history of fragility fractures, frailty, poor health, dementia, Caucasian or Asian race, calcium and vitamin D deficiencies, smoking, and excessive alcohol consumption. Moreover, certain diseases, such as rheumatoid arthritis, diabetes mellitus, and renal disease, as well as any kind of prolonged immobilization, can increase your risk of generalized osteoporosis and fractures. Furthermore, taking certain types of drugs, such as glucocorticoids, immunosuppressants, anticonvulsants, and testosterone antagonists, constitutes a risk factor for the disease. It is best to try to identify all of your risk factors before a fracture occurs.
Evaluation
Since an orthopedic surgeon is the first, and often the only, physician you may see if you break a bone, it is important that he or she have you evaluated for osteoporosis. Your evaluation should include a medical history, physical examination, laboratory tests, bone mineral density tests, and possibly x-rays. Although your orthopedic surgeon will typically initiate this evaluation while overseeing the care of your fracture, you may be referred to your primary care physician or a bone health clinic to treat the underlying causes of the disorder to prevent future fractures.
Treatment
As a fragility fracture patient, optimal care will involve not only treating your injury, but also identifying and treating the underlying cause. If your diagnosis is that you have osteoporosis, your treatment will begin with counseling about diet, exercise, and fall prevention. You may be encouraged to perform regular weight-bearing exercises, such as walking, and to get sufficient amounts of calcium (1,200 mg/day) and vitamin D (800 IU/day) through your diet, dietary supplements, and exposure to sunlight. Your treatment plan may also include pharmacologic agents to prevent bone loss, such as bisphosphonates, or various hormone therapies such as selective estrogen receptor modulators, parathyroid hormone, and calcitonin.
Fracture care
When it comes to fragility fractures, both nonsurgical and surgical management have proven highly successful, depending on the particular fracture. As with other types of fractures, the basic principle for the management of fragility fractures is to first reduce the fracture (manipulate the broken bone back into its proper position); next hold the fracture in this position (non-surgically with a splint or cast, or surgically with plates, screws, or rods); and, finally, to rehabilitate the patient through exercise and physical therapy. Sometimes, in order to provide extra support for weak bone, special techniques can be done surgically to create a more robust fixation construct. An example of this is the use of special locking screws. Additionally, after surgery you may be instructed to avoid weight bearing on the affected extremity for an extended period of time in order to help it heal.
Outcomes
You can both reduce your risk level and enhance outcomes for fragility fractures if you and your physician assume an active role in managing your osteoporosis and preventing additional fractures. While it is best to start a preventative program early (around age 30), it’s never too late to take care of your bones and improve your odds.
Author: Aaron D. Schrayer, MD | Lewisville, TX
Reprinted with permission from the Hughston Health Alert, Volume 28,Number 4, Fall 2016.
Last edited on October 18, 2021